
Plantar Fasciitis
Plantar fasciitis is one of the most common diagnoses that I see in the clinic. It can be quite debilitating and affect day to day life. What exactly is this fasciitis, and how do you get rid of it?
What is it?
Plantar fasciitis is an “itis” (or inflammation) of the plantar fascia band.
This plantar fascia band runs from the heel to the ball of the foot. It acts like a pully for the medial arch (largest and inside arch) of the foot. As you progress through your walking stride, the band will mechanically tighten and relax, which is dependent on how the joints are moving in the foot. It is NOT a muscle, which means it cannot contract to move joints.
When the band becomes injured, it can be from various situations. As a Pedorthist, I focus on how the foot affects the rest of the body. So, how does the foot affect the plantar fascia?
Causes
A common foot type causing plantar fasciitis is pes planus, which means flat foot. While standing with a flat foot, much strain occurs to the plantar fascia. 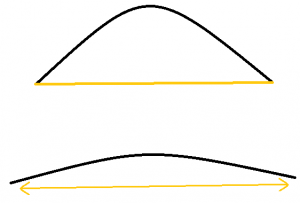 Think of it like an elastic band: this elastic band attaches on either side of a semi-circle. When this semi-circle flattens out, the elastic band stretches to allow this to happen. If you stretch this band a little bit in either direction, it returns to its original shape without damage. But, if it stretches even farther, you start to see damage to the elastic, which may break if stretched too far. If consecutively stretched 5000 times a day, the damage will be more apparent over time.
Think of it like an elastic band: this elastic band attaches on either side of a semi-circle. When this semi-circle flattens out, the elastic band stretches to allow this to happen. If you stretch this band a little bit in either direction, it returns to its original shape without damage. But, if it stretches even farther, you start to see damage to the elastic, which may break if stretched too far. If consecutively stretched 5000 times a day, the damage will be more apparent over time.
The difference in the elastic compared to the plantar fascia, is that the body adapts and can repair itself. The plantar fascia should be moving constantly while walking, but the body needs to be able to repair any small damage without any notice to the outside observer. Once the damage becomes so severe that the body cannot keep up with the repair, that is when plantar fasciitis begins.
At the other end of the foot spectrum there is pes cavus, which means high arch. This foot type is less common, but can still lead to plantar fasciitis. A high arch causes a tight plantar fascia band, and any movement can lead to strain. If the foot does not move, it prevents shock absorption during walking, and this shock may be absorbed by the plantar fascia band instead.
Other types of feet may not specifically fall into one of these two categories, but may have other factors causing plantar fasciitis. An example would be overpronation, which can be explained very similar to the relationship between pes planus and plantar fasciitis.
What will I feel?

Plantar fasciitis can be felt as pain at any point in the band. The most common areas are directly under the medial arch and a specific area in the heel. This area in the heel is the point where the plantar fascia attaches to the heel bone (calcaneus). It is located on the inside of the heel, and closer to the arch.
Early stages of plantar fasciitis exhibit as morning pain, that disappears after a few minutes of walking. This can develop into pain at the end of the day, pain while walking after a period of sitting, and eventually it can become constant pain throughout the day. This can also lead to a bone spur, which you can learn about in the February 2019 blog post.
Why did I get plantar fasciitis now?
There are many factors that contribute to the onset of plantar fasciitis. These factors can be a change in activity, footwear related, or even just an accumulation over time.
Activity changes can be related to changes such as intensity, duration, frequency, or type. A common change is a goal to lose weight, and the activity happens too fast for the plantar fascia to heal itself. Some will jump into a sport they haven’t played in years, and try to play at the same level as they did when they were in top shape for that specific sport.
Improper footwear commonly leads to plantar fasciitis, especially when worn for extended weight bearing activities such as on vacation, at an event, or starting a new job. Shoes do not last forever, and need to be replaced once their lifespan has expired. Running shoes are great for foot health, but once they break down, they can change they way your foot is moving.
Some people develop plantar fasciitis with no explanation to why it could have happened. Over time, the repair of the plantar fascia may be lagging behind very slowly, and eventually the damage overpasses the repair.
How do I reduce the pain?
There any many treatments and modalities to help with plantar fasciitis. The pedorthic intervention involves treatments such as stretching, icing, bracing, and orthotics.
Stretching and icing are a great way to help with the healing process, but they must be done consistently. Calf stretches and pulling the toes up to stretch the bottom of the foot are good places to start. Physiotherapists specialize in this area, and would have other treatment modalities to help.
Bracing may also help with the healing process, and in some cases prevent plantar fasciitis from returning. A night splint is worn at night to stretch the plantar fascia while sleeping. It reduces the morning pain of plantar fasciitis by allowing the plantar fascia to heal in the stretched position instead of relaxed. There are some braces that help lift the medial arch while walking, and may assist in preventing the return of plantar fasciitis in mild cases.
 Over the counter and custom orthotics help the healing process and to prevent the plantar fasciitis from returning. The orthotics support the arch, and other joints in the foot, to prevent excessive strain to the plantar fascia band.
Over the counter and custom orthotics help the healing process and to prevent the plantar fasciitis from returning. The orthotics support the arch, and other joints in the foot, to prevent excessive strain to the plantar fascia band.
Plantar fasciitis is a treatable condition that should not be ignored. If it sounds like the condition you have, or you would like more information, let us know!
You must be logged in to post a comment.

Comments (2)
Pingback: Bone Spurs in the Foot - the what, why and how | On the Ball Orthotics
Pingback: Other Forms of Heel Pain | On the Ball Orthotics, Barrie ON